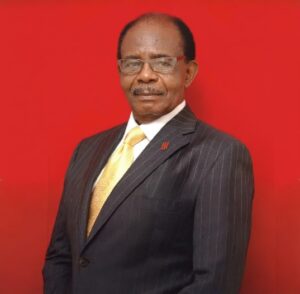
A Lifeline in Crisis: Why Prof. Idia Ize-Iyamu’s Intervention at UBTH Matters

By Orobosa Omo-Ojo JP
With tensions escalating at the University of Benin Teaching Hospital (UBTH), the situation is no longer merely administrative—it has become clinical, urgent, and potentially fatal.
At this critical juncture, the intervention of the Chief Medical Director, Prof. (Mrs.) Idia Nibokun Ize-Iyamu, stands as a defining moment in the hospital’s recent history.
This is why her actions deserve serious consideration and measured recognition.
The ongoing disagreement started during the industrial action by the Joint Health Sector Unions (JOHESU), when emergency services reportedly faced disruption. While labor disputes are part of institutional life, healthcare operates under a different ethical weight—where interruption can mean irreversible consequences.
According to a UBTH management source, a “Lifeline Agreement” was reached with striking workers during the industrial action to preserve emergency laboratory operations.
“Yet when implementation faltered, the responsibility to prevent system collapse shifted squarely to leadership.
“In crisis environments, leadership is not theoretical—it is practical. It requires decisions under pressure, often without the comfort of consensus,” the management source volunteered.
The controversial A&E Laboratory decision was taken by Prof. Ize-Iyamu to have a complementary private laboratory service within the Accident & Emergency (A&E) Unit to save more lives when union members failed to honour their ‘Lifeline Agreement.”
However, unionists framed the move as unnecessary or suspect. Emergency medicine relies on immediate blood grouping and cross-matching; rapid electrolyte and metabolic panels.
There is also a need for timely infection markers, and quick turnaround coagulation profiles. In such settings, minutes are clinically significant.
In defense of Prof Ize-Iyamu, the UBTH management argues that the decision to support the hospital diagnostic services with a private outfit, has complied with the Federal Ministry of Health directives. They added that it was designed to augment—not replace—existing UBTH laboratories, as more than ten of such continue to operate across the hospital.
Professionals have strengthened the management position that, if emergency diagnostics fail during critical windows, outcomes can deteriorate rapidly. The A&E laboratory, therefore, can be viewed as a continuity mechanism rather than a structural takeover.
In the emerging scenario, ethical obligation must outweigh institutional politics. It must also be noted that healthcare leadership carries a dual responsibility—protect staff welfare while at the same time, safeguarding patient survival. When these two interests collide, ethical doctrine traditionally prioritizes the vulnerable patient.
Reports from the hospital reveal cases where blood bank access became constrained during health workers strike periods and critical laboratory tests experienced delays.
The medical oath or the ‘Hippocratic Oath’ is a foundational pledge by health workers to uphold specific ethical standards, including beneficence, and non-maleficence. To this end, emergency care requires administrative intervention—which Prof. Ize-Iyamu has promptly done.
While independent verification remains important, the broader principle is clear—no hospital should allow emergency services to hinge entirely on industrial negotiations.
Prof. Ize-Iyamu’s intervention signals an attempt to decouple life-saving diagnostics services from labour volatility.
Prof. Ize-Iyamu is risking her reputation for continuity to ensure a paradigm shift from sloppy public health institution to a reliable life-saving regime.
Leadership decisions that disrupt entrenched systems often provoke backlash, it is not surprising that entrenched interest groups within and outside UBTH have taken to the social media campaign to discredit the reforms.
The ongoing campaign against the management of UBTH demonstrates how swiftly narratives can shift in the digital age. But it must be noted that reform frequently carries reputational risk.
By authorizing structural adjustments during a tense labour climate, the Chief Medical Director, Prof. Ize-Iyamu has exposed herself to criticism, public scrutiny, and institutional resistance. That willingness to absorb personal and professional heat in order to preserve service continuity reflects a calculated prioritization of patient welfare.
The broader healthcare reality is that, public tertiary hospitals like UBTH are operating under immense strains—including increasing patient loads; limited federal allocations; high referral complexity; equipment maintenance challenges and workforce disputes.
In such ecosystems, stability depends on proactive management, and system sustainability sometimes requires unpopular decisions—especially when infrastructure vulnerabilities are exposed during crises.
A major remedy for these challenges include price adjustments, operational restructuring, and outsourcing of complimentary services and these are not automatically evidence of misconduct.
They may reflect attempts to stabilize fragile systems and prevent recurrence of service paralysis. Along this line of thought, Prof Idia Ize-Iyamu’s action is a ‘Preventive Model for the Future’.
The long-term significance of the A&E laboratory intervention lies in its preventive value. If emergency diagnostics are insulated from future strikes or departmental disruptions, the hospital reduces its exposure to catastrophic downtime that may turn the hospital to a killing field.
Healthcare institutions globally, adopt contingency frameworks precisely to prevent single points of failure, in that light, Prof. Ize-Iyamu’s actions can be interpreted as institutional risk management action, rather than administrative overreach.
And beyond personalities, is the question of ‘Duty’.
Ultimately, the moment in UBTH transcends personalities and internal rivalries. It centers on a foundational question: When faced with the possibility that critical services could be halted, should hospital leadership wait—or act?
Prof. Idia Ize-Iyamu chose to act.
Her intervention reflects a view of leadership rooted in oath-bound responsibility: that the pulse of a hospital must not stop, regardless of internal turbulence. As UBTH continues navigating reform, scrutiny and transparency remain essential.
But so too does acknowledgment of decisive leadership when continuity of life-saving care hangs in the balance.
In healthcare, history often judges leaders not by how well they avoided controversy—but by whether patients survived the storm. The systematic maleficence at the University of Benin Teaching Hospital must give way to life-saving changes urgently needed in the federal institution.